A newly discovered communication pathway linking far-flung nerve centers within the brain and skull, and the body beyond, could provide a new target to stop migraine pain in its tracks.
Researchers have long tried to pinpoint where migraines begin in the brain, and how these one-sided, nauseating headaches induce pain and other symptoms, such as vomiting. Understanding this would help find new ways to prevent migraines from happening or at least ease the searing pain once it starts.
For one-third of people who experience migraines, these are preceded by an aura, a shimmering light or blurring of vision that is itself foreshadowed by a wave of abnormal brain activity that spreads through the cortex, the outer layer of the brain.
But how this activity inside the brain affects receptors on pain-sensing neurons outside it has remained a little fuzzy.
The brain is wrapped in a protective layer, the blood-brain barrier, which keeps potentially harmful substances and pathogens out of the central nervous system (CNS). The spinal cord has its own cocoon too, which also stops large molecules from passing through.
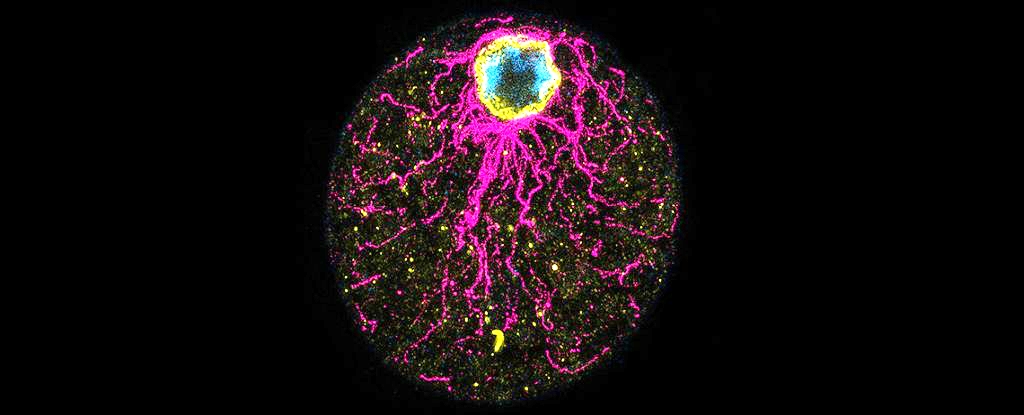
One key nerve hub linking the CNS to all the nerves outside it – the peripheral nervous system – is the trigeminal ganglion. Already implicated in migraines and headaches, this bean-shaped cluster of nerves is located at the base of the skull and transmits sensory information from the face and jaws to the brain.
Researchers thought the trigeminal ganglion sat outside the blood-brain barrier, which conveniently meant it could be an easier target for drugs, such as CGRP inhibitors, a promising new type of migraine therapy.
However, this positioning implied that the trigeminal ganglion was not exposed to the cerebral spinal fluid (CSF) that bathes the brain and spinal cord.
The new study in mice shows quite the opposite: It revealed CSF carries signaling molecules directly to cells in the trigeminal ganglion, bypassing a slower, known route through the meninges, a triple-layered membrane enveloping the brain and spinal cord.
“We identify a communication pathway between the central and peripheral nervous system that might explain the relationship between migrainous aura and headache,” University of Copenhagen biologist Martin Kaag Rasmussen and colleagues explain in their published paper.
In a series of real-time imaging experiments, the researchers traced the flow of CSF from the visual cortex of the brain, the most common site of migraine aura, to the trigeminal ganglion in mice.
The fluid rapidly entered the root of the trigeminal ganglion, which further dissections showed lacks a tightly wrapped sheath that bars dissolved molecules from penetrating the trigeminal nerves any further along their spindly bodies.
What’s more, molecules dissolved in the CSF from one hemisphere of the cortex flowed primarily to the trigeminal ganglion on the same side of the head, which could explain why migraines tend to be one-sided.
Rasmussen and colleagues also found the contents of the animals’ CSF were altered after an aura; it contained CGRP (calcitonin gene-related peptide) and other molecules released from the cortex after a wave of abnormal brain activity passed through, with those molecules activating trigeminal ganglion nerves.
“Our observations indicate that the trigeminal CSF uptake drives the immediate migraine headache,” Rasmussen and colleagues write. However, “we also found that CSF composition quickly normalizes, suggesting that other processes might drive headache at later phases.”
There are some obvious differences between mice, humans, their brains and migraines, too. Still, the researchers hope that identifying this new signaling pathway “may enable the discovery of new [drug] targets, to the benefit of the large portion of patients not responding well to currently available therapies.”
Already, their findings suggest CSF is much more than a simple fluid flushing out the body’s ‘waste clearance system’, and is instead an important signal carrier. However, there’s a lot we’re still discovering about fluid flows in the brain.
“Together, these findings provide a new mechanism that links the central and peripheral nervous systems,” neuroscientists Andrew Russo, of the University of Iowa, and Jeffrey Iliff, at the University of Washington, write in a perspective accompanying the study.
“Similarly, this mechanism may explain the intermingled clinical associations between traumatic brain injury, sleep disruption, and posttraumatic headache.”
The study has been published in Science.