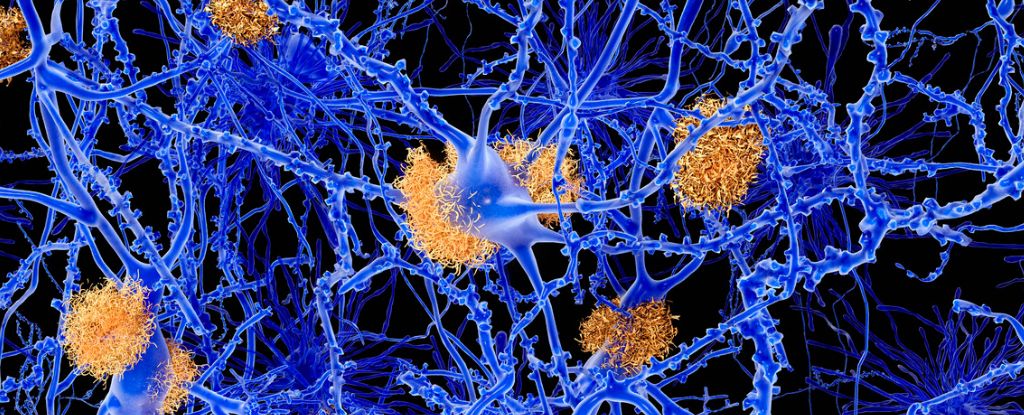
Neurons aren’t the only brain cells producing the proteins associated with Alzheimer’s disease, a new study of mouse models reveals. It turns out that cells supporting neurons contribute to this process too.
Amyloid beta proteins occur naturally in our brains, but have long, and now controversially, been associated with Alzheimer’s disease.
“Until now, neurons were thought to be the main producers of amyloid beta and have been the main target for new drugs,” says molecular biologist Klaus-Armin Nave from the Max Planck Institute for Multidisciplinary Sciences in Germany .
Treatments targeting these proteins have not been as successful as hoped, indicating we’re still missing crucial components of this disease.
The fact that there are other contributors to amyloid beta clumps may provide some sorely needed clues.
With a new dementia diagnosis now being made every three seconds, more and more of us face the frightening symptoms of confusion, communication difficulties, and memory loss personally or in our loved ones.
Max Planck neurogeneticist Andrew Octavian Sasmita and colleagues demonstrated the involvement of neuron support cells, oligodendrocytes, in abnormal brain plaque formation by removing their ability to create amyloid beta.
They did this by knocking out the gene behind beta-site APP cleaving enzyme 1 (BACE1). As its name suggests, BACE cleaves amyloid-beta precursor protein (APP), which is involved in producing amyloid beta.
“Oligodendrocytes lacking BACE1 developed about 30 percent fewer plaques,” explains Max Planck neurogeneticist Constanze Depp.
While inhibiting BACE1 generally has a far greater reduction in plaque formation (over 95 percent) in mice, BACE inhibition appears to cause other debilitating problems including worsening memory and brain volume declines in human clinical trials.
This is likely because BACE1 is involved in the proliferation of neurons in adult mice. But when Sasmita and team knocked out BACE1 within just oligodendrocyte cells, they found no disruption in neuron amounts or their distribution.
“Potentially, selective targeting of BACE1 in oligodendrocytes could spare the detriments of widespread BACE1 inhibition,” the researchers write in their paper.
Other researchers now caution that a continued focus on amyloid beta proteins may be keeping us stuck on the wrong path, as these plaques may just be a side effect rather than causing Alzheimer’s.
However, previous research has implicated oligodendrocytes in Alzheimer’s disease too.
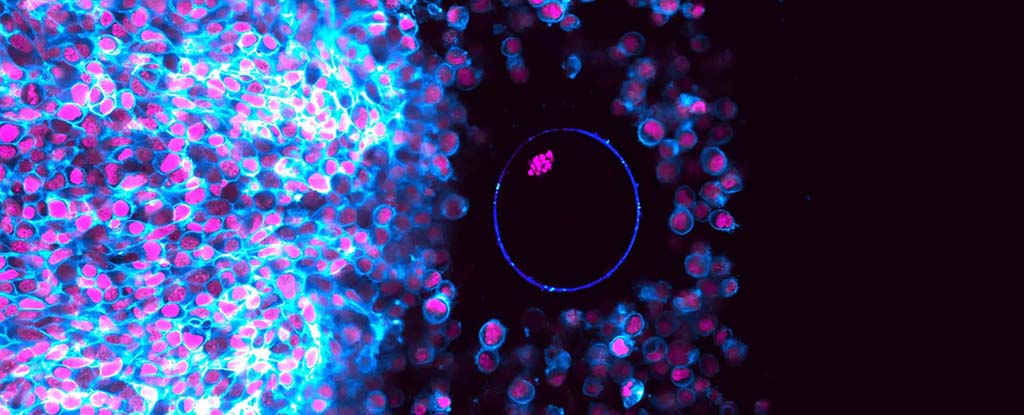
“One of the tasks of oligodendrocytes is to form myelin – an insulating layer – and wrap it around the nerve fibers to speed up signal transmission,” explains Sasmita.
This process also seems to be going awry in mouse models of Alzheimer’s, suggesting that even if amyloid beta ends up being a dead end, oligodendrocyte cells may still be playing a role in causing this stubbornly incomprehensible disease.
This research was published in Nature Neuroscience.