Every 30 seconds, someone in the world will experience a flare-up of their asthma or chronic obstructive pulmonary disease (COPD) symptoms.
For decades, the standard treatment for these potentially life-threatening episodes has remained unchanged – treatment with steroids, such as prednisolone.
Unfortunately, these drugs don’t work for everyone and they have significant levels of serious side-effects. Nearly one-third of patients treated with steroids will see their symptoms worsen again within a month, requiring more treatment and increasing the risk of side-effects.
But what if there was a better option?
Our latest study, published in The Lancet Respiratory Medicine, has revealed that a drug called benralizumab – administered as an injection – may be the breakthrough that we have been waiting for.
The results suggest that this treatment, administered at the time of a flare-up, is highly effective and spares patients the side-effects of steroids.
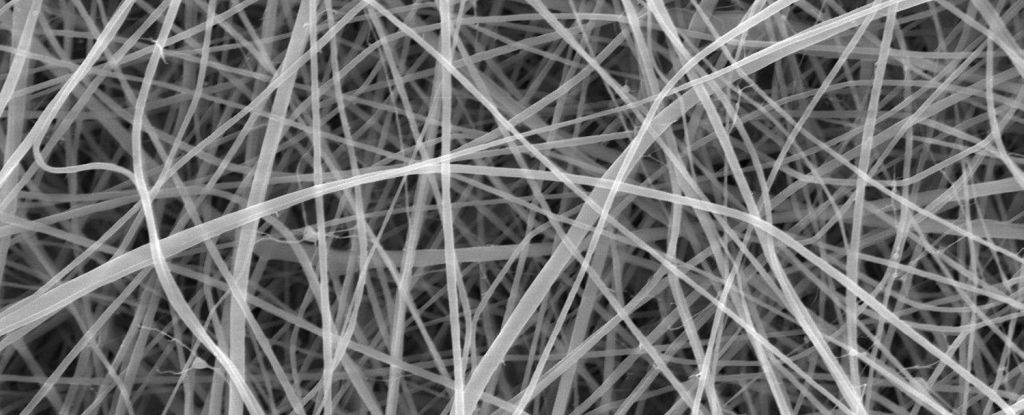
Inflammation caused by a type of white blood cell called eosinophils is a key driver of flare-ups in many people with asthma and some people with COPD. Eosinophilic inflammation plays a role in at least half of asthma and one-third of COPD flare-ups.
For these people, targeting eosinophils when symptoms worsen is a promising strategy.
Benralizumab, a monoclonal antibody, is already used for the long-term management of eosinophilic asthma, with studies still evaluating the effect for long-term management in eosinophilic COPD.
However, the potential to manage critical moments, when symptoms suddenly worsen, had not been studied before.
In the trial, 158 patients experiencing asthma or COPD flare-ups were recruited from two UK hospitals. Participants were randomly assigned to one of three groups: standard treatment with prednisolone tablets, a single injection of benralizumab alone, or a combination of the two.
Striking results
The main outcome we were interested in was the “rate of treatment failure”, defined as the need for further therapy, hospitalisation or death, within 90 days.
The results were striking: 74% of those treated with prednisolone alone experienced treatment failure within 90 days. Failure rates dropped to 47% with benralizumab alone and 42% with the combination therapy.
Pooled data from the benralizumab-treated groups showed that only 45% of patients experienced treatment failure, compared with 74% in the prednisolone group. For every four patients treated with benralizumab, one treatment failure was prevented.
The benefits of benralizumab extended beyond treatment failure rates. Patients treated with benralizumab reported faster symptom recovery and improved quality of life. For example, patients were able to breathe better and had less discomfort.
Benralizumab also had a better safety profile compared with prednisolone. Side-effects commonly linked to prednisolone, such as high blood sugar, were absent in patients who received benralizumab alone.
This makes the therapy especially promising for people who face significant risks from repeated prednisolone use, such as older adults and those with diabetes or osteoporosis.
While a lower dose of benralizumab is already approved for long-term asthma management, it is not yet licensed for use during flare-ups at the dose used in this study.
For that to happen, phase 3 trials will be needed, involving more diverse and international populations. (Phase 3 is the final phase of testing in humans before a drug is approved.)
If these trials confirm the findings, benralizumab could become the first new therapy approved for eosinophilic exacerbations of asthma and COPD in over 50 years.
In the time it has taken you to read this article, 40 people in the world have experienced an eosinophilic asthma or COPD flare-up. Under current best treatments, 30 of them will require further care within 90 days.
Benralizumab offers the potential to break this cycle of recurrent treatment and side-effects, transforming the way we manage these common and debilitating conditions.
Could this drug be the breakthrough we’ve been waiting for? The early evidence suggests it just might be.![]()
Mona Bafadhel, Chair of Respiratory Medicine, King’s College London; Richard Russell, Clinical Reader, Respiratory Medicine, King’s College London, and Sanjay Ramakrishnan, Clinical Senior Lecturer and Respiratory Physician, The University of Western Australia
This article is republished from The Conversation under a Creative Commons license. Read the original article.