A highly common bacterial affliction that impacts nearly a third of women worldwide could very well be an overlooked sexually transmitted infection (STI).
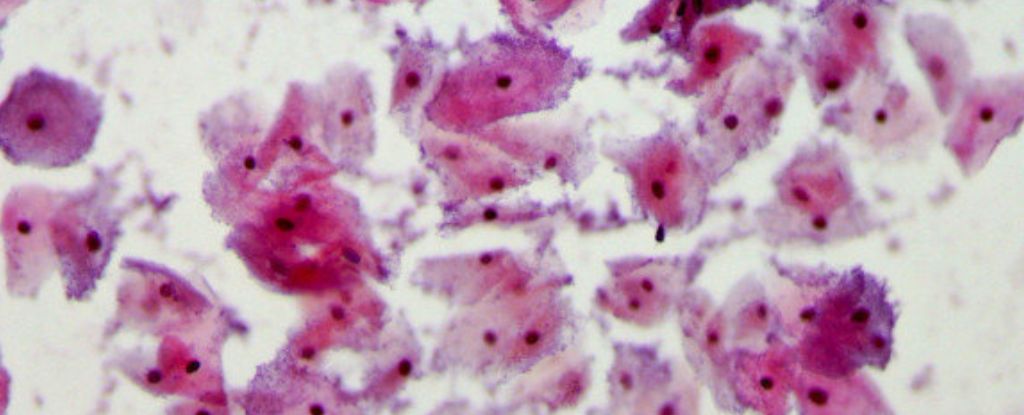
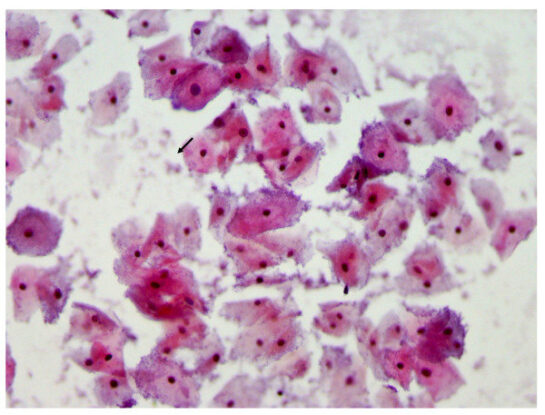
Bacterial vaginosis (BV) occurs when the vaginal microbiome hosts an increase in some harmful bacteria and a decrease in protective species, which can lead to an unpleasant ‘fishy’ smell, abnormal vaginal discharge, burning, or itching (although many have no symptoms at all).
In the past, scientists have argued that BV doesn’t meet the requirements of an STI because the bacteria come from within. But that may not be true in all cases.
While BV is considered both treatable and curable, some scientists have pointed out there is an “unacceptably high proportion” of women (around 50 percent) experiencing BV recurrence within 6 months of taking a week-long antibiotic, leaving them vulnerable to risks of infertility, premature births, and low birth weight for infants.
Previous studies have found that men also harbor bacterial species associated with bacterial vaginosis in the distal urethra and the penis, and the risk of BV recurrence in women doubles if they have a regular sexual partner.
A new randomized trial from Australia suggests we need a revolution in how BV is treated. The findings reveal that regular male partners can re-seed BV infections during sexual activity if they are not treated as well.
“Our trial has shown that reinfection from partners is causing a lot of the BV recurrence women experience, and provides evidence that BV is in fact an STI,” says clinician scientist Catriona Bradshaw from Monash University.
If the authors are right, and BV really is an STI, then it could be one of the most common in the world. For perspective, the lifetime risk of chlamydia, which is currently the most common STI, impacts about 1 in 5 women in some parts of the United States.
Sexual activity is considered a main risk factor for BV, and yet infectious disease specialists Jack Sobel and Christina Muzny, who were not involved in the current research, explain that “bacterial vaginosis is still unfortunately not accepted as an STI by practitioners.”
Virtually all previous studies that have treated male partners for BV have failed to show reduced recurrence rates in their female partners, and yet often, these trials have treated men using only an oral tablet. This may not be enough to quash the infection completely.
The new trial is the first of its kind to show that simultaneously giving oral and topical antimicrobial treatments to male partners of women who are also receiving first-line BV therapy reduces the risk of recurrence 12 weeks later.
The study split 164 heterosexual, monogamous couples in which the woman had BV into two groups. In the first group, only women were treated for BV using antimicrobial agents, following current global recommended practice. In the second group, the women were treated and the men were also given an oral antibiotic and a topical clindamycin cream to apply to the penile skin.
At 12 weeks, BV recurrence was documented at 35 percent in the partner-treatment group, as opposed to 63 percent in the group that treated just women.
The findings suggest that current standard care for BV is not cutting it and can be greatly improved upon.
“This successful intervention is relatively cheap and short and has the potential for the first time to not only improve BV cure for women, but opens up exciting new opportunities for BV prevention, and prevention of the serious complications associated with BV,” says Bradshaw.
Further research will be needed to test this approach on larger and more diverse cohorts, but the findings suggest that condoms aren’t the only way to reduce the possibility of BV sexual transmission.
“This trial provides data critical to educating clinicians and patients about the role of sexual transmission of bacterial vaginosis–associated bacteria and the benefit of male-partner treatment,” write Sobel and Muzny.
“It is time to start the conversation.”
The study was published in the New England Journal of Medicine.