Doctors in the UK have welcomed a breakthrough treatment for an aggressive form of leukemia after a teenager became the first patient to be given a new therapy and went into remission.
The 13-year-old girl, identified only as alyssawas diagnosed Acute T-cell lymphoblastic leukemia in 2021.
But her blood Cancer have not responded to conventional treatment, including chemotherapy and a bone marrow transplant.
She was enrolled at a clinical study of a new treatment at London’s Great Ormond Street Hospital for Children (MY GOODNESS) with genetically engineered immune cells from a healthy volunteer.
After 28 days, her cancer was in remission, allowing her to receive a second bone marrow transplant to restore her immune system.
frameborder=”0″ allow=”accelerometer; autoplay; write clipboard; encrypted media; gyroscope; picture-in-picture” allow full screen>
Six months later, at home in Leicester, central England, she is “fine” and receiving follow-up care.
“Without this experimental treatment, Alyssa’s only option was palliative care,” the hospital said in a statement Sunday.
Robert Chiesa, a GOSH consultant, said Their turnaround has been “quite remarkable,” although the results will need to be monitored and confirmed over the next few months.
cutting edge
Acute lymphoblastic leukemia (ALL) is the most common type of cancer in children and affects cells in the immune system, known as B cells and T cells, that fight and protect against it viruses.
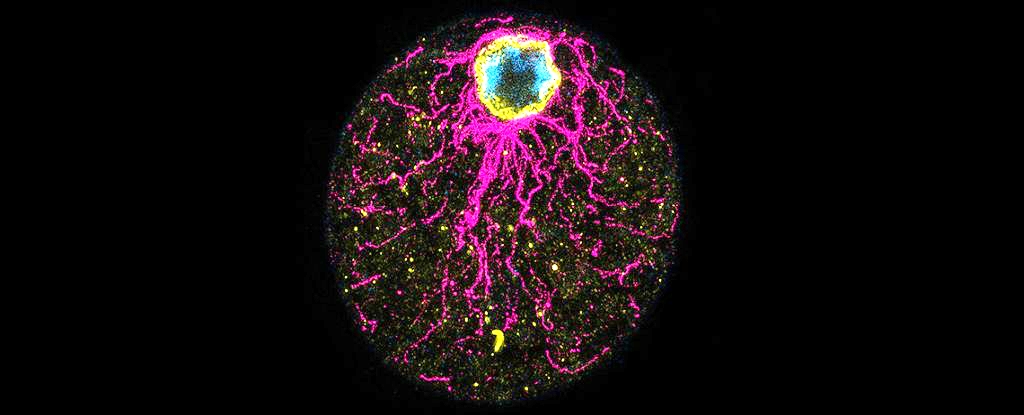
GOSH said Alyssa is the first known patient to have been given her base-edited T cellsin which individual nucleotide bases – letters of the DNA code – that contain instructions for a specific protein are chemically transformed.
Researchers from GOSH and University College London helped develop the use of genome-edited T cells to treat B-cell leukemia in 2015.
However, to treat some other types of leukemia, the team had to overcome the challenge that T cells, which are supposed to recognize and attack cancer cells, had killed each other during the manufacturing process.
Several additional DNA changes were required on the base-edited cells so they could target cancer cells without damaging each other.
“This is a great demonstration of how, with expert teams and infrastructure, we can combine cutting-edge technologies in the laboratory with real outcomes in the hospital for patients.” said GOSH Consulting Immunologist and Professor Waseem Qasim.
“It is our most advanced cell engineering to date and paves the way for other new treatments and ultimately a brighter future for sick children.”
Alyssa said in the statement she was encouraged to take part in the process not only for herself but for other children as well.
her mother, Kiona, added: “Hopefully this can prove that the research works and they can offer it to more children.”
The researchers presented their findings this weekend at the annual meeting of the American Society of Hematology.