A new study in Japan has once again raised questions about the relationship between oral health and brain health; which most experts agree are surprisingly interconnected.
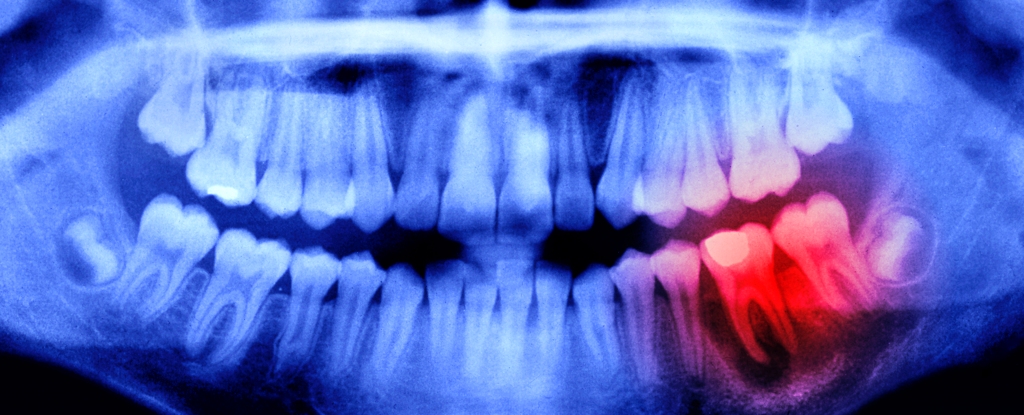
It investigated whether problems in the mouth like periodontitis (gum disease) and tooth loss can increase the risk of neurodegenerative disorders like stroke, Alzheimer’s, and other forms of dementia.
The results were clear: both issues are associated with a faster rate of atrophy in the hippocampus – the part of the brain that governs memory, learning, and emotion. This is a significant result, however it is not the first time such a link has been made.
In March, a US study of more than 40,000 adults enrolled in the UK Biobank research project found that poor oral health appears to be a key risk factor for stroke and dementia.
In a 2019 literature review, another set of researchers concluded that “collectively, experimental findings indicate that the connection between oral health and cognition cannot be underestimated”.
This growing body of research has huge implications both for our understanding of the body, and for preventative intervention strategies in public health.
Satoshi Yamaguchi, lead author of the Japanese study, has reflected on his findings: “retaining more healthy teeth without periodontal disease may help to protect brain health… Regular dental visits are important to control the progression of periodontal disease.”
In other words, it is not enough to simply maintain a full set of teeth to stay healthy. We must also keep our mouths free from periodontal disease, or else the brain could suffer the cost.
This is not a mere academic concern. The World Health Organization estimates that severe periodontal disease, characterized by bleeding/swollen gums and damage to the supporting tissue of the teeth, impacts about 19 percent of the global adult population.
For context, this means more than 1 billion people could be at risk of early cognitive decline due to the state of their mouths.
Worse, the nature of the relationship between the mouth and brain appears to be bidirectional, meaning that cognitive decline tends to lead to poorer oral health habits as well.
Indeed, neurologic disorders like Alzheimer’s can make it difficult to properly care for the teeth. People with cognitive decline may forget to brush, or may struggle to cope with routine trips to the dentist. The result can be a vicious circle in which cognitive decline leads to a fall in dental standards, which only exacerbates the condition.
To prevent this snowball effect, policymakers and health experts must intervene early to nip the problem in the bud.
By emphasizing the value of brushing, flossing, visiting the dentist, and making sound dietary choices wherever possible, they can help older people to safeguard their mouths against plaque and bacteria – and hence reduce the risk of neurodegenerative disease.
Equally, for those who are already showing signs of dementia, families and caregivers can help dementia patients build a robust oral health routine tailored specifically to them.
This might involve scheduled reminders on the phone to brush and floss, or providing specialist dental tools like electric toothbrushes – which can be easier to operate. Some dentists even offer home visits for dementia patients that struggle to attend appointments on their own.
Encouraging patients to adopt other preventative habits, such as using sugar-free chewing gum between meals, might also have an impact. Research suggests that regularly chewing SFG (alongside brushing) can help reduce the risk of cavities. It is also easy to leave packets of gum lying around in eyesight of patients, negating the need for constant reminders to start chewing.
These kinds of small, consistent lifestyle changes can make a huge difference over time, and they are considerably easier to maintain than more infrequent and intrusive dental interventions.
The fact is, given the considerable impact of poor oral health on the wider body (including the brain), we simply cannot afford to keep treating dental care as a second-order concern. Preventative measures are a crucial part of maintaining the long-term integrity of the teeth and gums, and dementia patients should be supported to do this wherever possible.
Of course, the battle against conditions like Alzheimer’s cannot be reduced solely to oral health. Many factors contribute to the onset of dementia, and it would be wrong to overstate the impact of the mouth on this process.
Nevertheless, the evidence is clear that oral health interventions can help in the fight against cognitive decline, and clinicians have a key role to play in spreading this message.
Dr Ben Atkins BDS is the Past President of the Oral Health Foundation and a general dental practitioner. He is also a long-standing Trustee for the charity, and owns a group of dental practices in the North West of England.