A simple tooth extraction ended in a trip to the emergency room with nausea, dizziness, and tilted vision for an Australian man in his 60s, who was later diagnosed with a rare disorder that causes blood vessels in the brain to wither.
Though it’s impossible to say for certain that the bleed and the dental procedure were linked, the authors of a recently published case study suspect a sharp rise in blood pressure was the trigger for what’s known in medical parlance as an intracerebral hemorrhage.
Even while in the emergency room, the patient’s blood pressure remained understandably high. With his eyes flicking strongly to the left, his gait wonky, and his posture leaning strongly to the right, it was clear something wasn’t quite right in the neurological department.
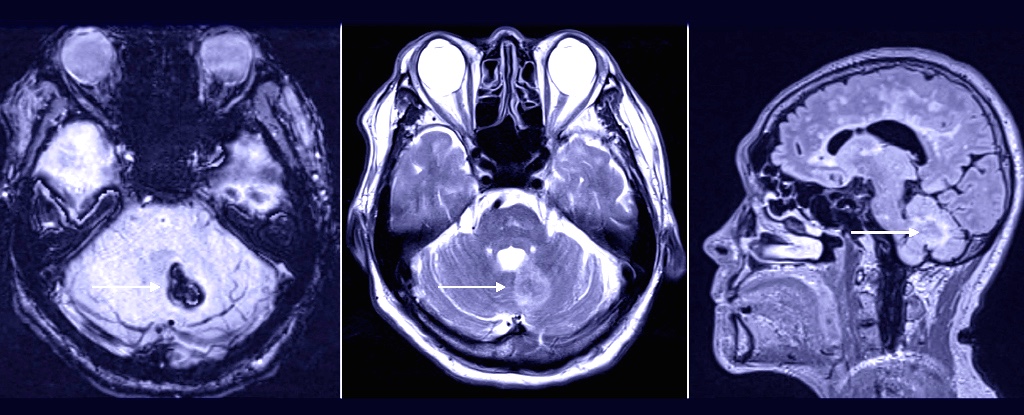
One of the first diagnoses to rule out in such cases is stroke. An urgent CT scan promptly revealed a small bleed putting pressure on tissues in the lower left half of the patient’s brain.
Being the vitally important organs they are, blood vessels feeding the brain don’t tend to simply leak willy-nilly. In fact, they’re well adapted to keep all but the most essential materials away from sensitive neurons and their support cells.
So identifying the cause of an intracerebral hemorrhage becomes a matter of high priority. Recently suspected of having Parkinson’s disease, the patient had a simple CT scan taken just six weeks earlier.
There were no obvious signs of concern as far as blood vessels went, though there were significant signs of something called white matter disease – a broad reference to damage to the brain’s supporting ‘white cells’ caused by reduced blood flow.
Using an MRI to get a more detailed look, the medical team mapped the areas and types of brain tissue affected. Once again, localized zones of white matter disease hinted at a deeper, more chronic pathology.
The acronym CADASIL – for cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy – describes a rare medical condition that affects the flow of blood through small vessels, particularly those weaving their way through brain matter.
Thought to affect as few as 2 out of every 100,000 people, the condition is typically missed or misdiagnosed, making it hard to know for sure just how common it might be.
Thanks to a mutated gene coding for special receptor proteins, muscles surrounding the blood vessels die prematurely, weakening the capillaries to the point of blockage. The end result is commonly leukoencephalopathy, or death of the brain’s white matter.
One DNA test for a broken NOTCH3 gene later and the patient had his diagnosis. Though he recovered from this bleed over the next few months, he was put on a long-term course of aspirin to keep his blood flowing more easily, and a medication to help control his blood pressure.
Blockages might be common in patients with CADASIL, but hemorrhages aren’t, at least compared with other stroke-causing abnormalities. In fact, this case study is the first to describe a brain bleed in a dental patient with CADASIL.
The medical literature only mentions three other cases of anybody experiencing an intracerebral hemorrhage while in the dentist’s chair. One case reported more than 30 years ago featured a 52 year old woman with a painful abscess, who unfortunately didn’t survive her substantially large intracerebral hemorrhage.
Before you whip out such rare examples of neurological trauma as an excuse to avoid your next check-up, it pays to keep in mind that the dentist is your brain’s best friend.
Having gum disease over a number of years could raise your risk of Alzheimer’s by as much as 70 percent. Similarly, having bad oral hygiene could shrink areas of your brain linked with memory.
Keep calm and say ‘ah’. Odds are good you’ll still be smiling in decades to come.
This research was published in BMJ Case Reports.
A version of this article was first published in August 2023.