The decades-long search for one HIV Vaccine has been dealt another major blow as the “last real candidate in development” is no better at preventing infections than a late-stage placebo clinical trials.
The multinational Mosaico study, which began in 2019 and involved more than 3,900 volunteers, evaluated a four-shot HIV vaccine for cis men and transgender people who have sex with cis men and/or transgender people.
As the US National Institute of Allergy and Infectious Diseases (NIAID) reported Last week, the study was halted after a planned data review by the study’s independent data and safety monitoring board found the vaccine to be safe but ineffective.
“To our research partners and others who have dedicated decades to developing vaccines to end HIV/ AIDS Pandemicthese results are disappointing,” said study leader Susan Buchbinder, an HIV researcher at the University of California, San Francisco. said in an opinion.
“Although HIV continues to present a unique challenge for vaccine development, the HIV research community remains fully committed and each study brings us one step closer to realizing this.”
The vaccine was developed by Janssen, the vaccines arm of Johnson & Johnson, who tested the same vaccine delivery system as their now widely used one COVID-19 Vaccination.
Despite Decades of researchTo date, only one vaccine candidate has shown even marginal efficacy in preventing HIV infection. CIt was completed in the early 2000s the largest HIV vaccine trial to date. Researchers hoped to improve these results with an HIV vaccine that offered broad protection.
Plus the Mosaico process and other parallel studiesstudied vaccines based on “mosaic” immunogens — snippets of genetic material from multiple HIV subtypes — designed to train the body’s immune system to recognize the broad array of global HIV strains.
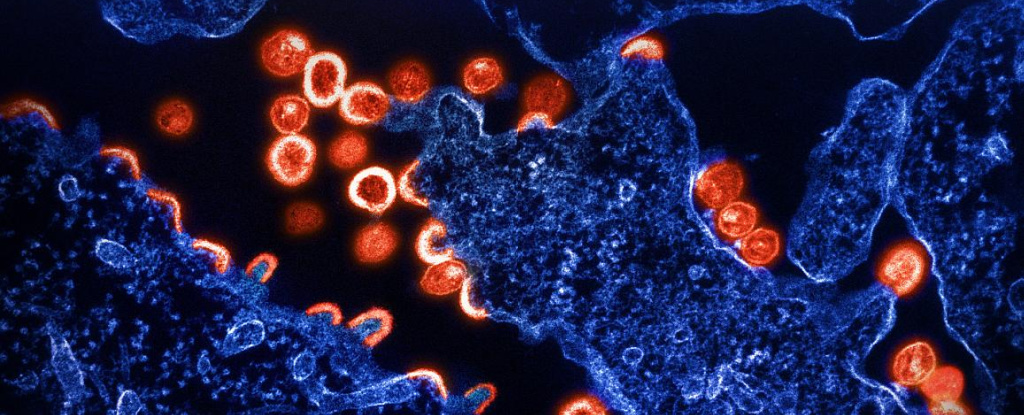
This was seen as a promising strategy against HIV, a notorious one virus that mutates rapidly and is effectively many steps ahead of vaccine development. It also shields itself from being recognized by antibody with a highly sugared protein coat.
When the process started, Buchbinder was said it is “an important step in the development of a safe and effective HIV vaccine for people worldwide”.
That feeling still rings true even when the process comes to an end. Experts | to say The way the study evaluated participants’ choices, removed barriers to access preventive medicines and included those most vulnerable to HIV will have lasting benefits.
Volunteers were only included in the study after being offered and refused antiretroviral drugs that can prevent HIV infection. These preventive drugs, called HIV Pre-Exposure Prophylaxis (PrEP), are taken daily. Those who chose to use PrEP were included in services that deliver the drugs, and study participants who later changed their minds and wanted to use PrEP were able to do so too.
“One thing we clearly learned from the study participants is that people want choice and that a vaccine will be an important option for those who don’t want PrEP,” says Buchbinder said.
“The ethical and community-friendly design and conduct of this study helped build trust in communities that may not be inclined to trust research organizations,” said Mitchell Warren, executive director of the AIDS Vaccine Advocacy Coalition, added.
Other efforts to develop HIV vaccines are continuing. Three mRNA HIV vaccines are available is currently being tested in a phase I clinical studywhich will examine whether the vaccines are safe and can stimulate an immune response.
“Finding an HIV vaccine has proven to be a daunting scientific challenge,” said immunologist and former NIAID director Anthony Fauci said in a statement last year.
“With the success of safe and highly effective COVID-19 vaccines, we have an exciting opportunity to learn if mRNA technology can produce similar results against HIV infection.”
The problem is that Phase I safety trials are a long way from Phase III trials, which provide data on whether or not a new vaccine (or drug) is effective. As such, it will be many years before we see another candidate make it to late-stage trials.
As Warren told For Stat News health reporter Helen Branswell, the latest study results are a “harsh reminder” of the challenges of developing an HIV vaccine.
At least five experimental HIV vaccines tested in nine studies have failed in efficacy studies, Warren said. He suspects the problem isn’t with the vaccine delivery systems — which have worked against COVID-19 — but with the immune targets that HIV vaccines are trying to hit.
“Our challenge is to figure out exactly what the goal is,” Warren told Branwell. “We have the vehicles. We don’t even know which passengers to put in the vehicles.”
A tough task against a changing virus.