Scientists have figured out a whole new way to cut the legs out from underneath drug-resistant bacterial infections.
The new class of antibiotic was identified by researchers at Uppsala University in Sweden, and while it has only been tested on mice, the team hopes that further development of the drug can “make an important contribution to the ongoing struggle against antibiotic resistance.”
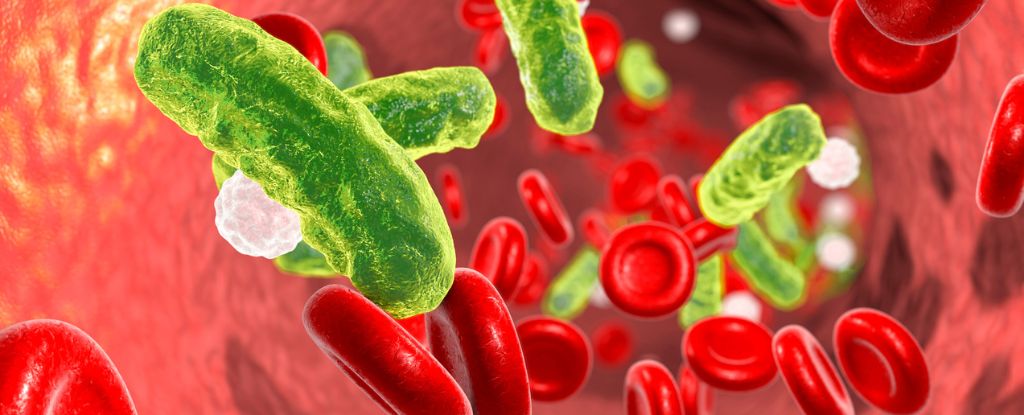
The unique medicine, like many other antibiotics currently in development, targets the double membrane that surrounds gram-negative bacteria, like Escherichia coli, which can cause bowel and blood infections, and Klebsiella pneumoniae, which can cause lung, bladder, and blood infections.
Unlike gram-positive bacteria, for which numerous families of drugs have been made, that formidable second barrier surrounding gram-negative bacterial cells makes it harder for antibiotics to have an effect.
The tough outer membrane is embedded with lipopolysaccharides, which give the cell integrity, allow it to interact with other surfaces, and permit the exit of toxins and the entry of nutrients.
For years now, scientists have tried to mess with the lipid membranes themselves, as they are essential to the functioning of gram-negative bacteria. But researchers in Sweden are the first to target an enzyme, called LpxH, which helps synthesize other critical components of the outer membrane called lipopolysaccharides. Since roughly 70 percent of gram-negative bacteria utilize this enzyme, it could make a suitable target for numerous infections.
Mice injected with drug-resistant E. coli or K. pneumoniae were dosed with an array of compounds an hour later designed to inhibit the bacteria’s LpxH. The results demonstrated it was possible to treat bloodstream infections in just four hours with just one dose.
“During the course of this infection model, bacteria spread to the bloodstream of the mice,” they explain.
“The ability of these compounds to strongly reduce the number of bacteria recovered from blood in only a single-dose treatment highlights their potential to treat the most life-threatening infections with gram-negative [multi drug resistant] pathogens.”
The researchers started with a compound called JEDI-1444, which was cobbled together from the results of a search through the literature for suitable candidate inhibitors. Though it showed incredible promise in preventing gram-negative growth, it wasn’t very soluable or stable in blood.
With a few modifications, the team found success in two variations coded EBL-3599 and EBL-3647, which were not dissolved better in serum but showed “potent” antimicrobial activity against a wide range of E. coli and K. pneumoniae isolates, “irrespective of the resistance genotype.”
That’s a critical discovery, given that both these bacteria are growing resistant to the few available antibiotics that do work against them. In 2019, death from antibiotic resistant infections was the third leading global cause of death. By 2050, ten million deaths are expected per year.
As bacteria adapt to our medicine, new classes of medicine are desperately needed to save lives. Today, half of the antibiotics available on the market are simply variations of drugs that were identified nearly a century ago.
In 2017, the World Health Organization (WHO) released a list of the most dangerous, drug-resistant pathogens and gram-negative bacteria that are resistant to the most effective classes of broad-spectrum antibiotics are top of the list. This includes E. coli and K. pneumoniae, Pseudomonas aeruginosa, which also causes pneumonia, and Acinetobacter baumannii, which causes blood, lung, and urine infections.
“While the current results are very promising,” researchers at Uppsala conclude, “there will be considerable additional work required before compounds of this class will be ready for clinical trials.”
The study was published in PNAS.