Your gut is likely littered with tiny particles of plastic, a now common condition in humans and many other animals around the world. The pieces are tiny, but they could pose an outsized threat to human health, researchers report in a new study.
By testing how microplastics Effects on human gut organoids (small, self-assembling tissue cultures that mimic real intestines) researchers found evidence of possible inflammatory effects, including the release of human-related cytokines inflammatory bowel disease (IBD).
This is important, researchers explain, because while we know that microplastics (along with even smaller nanoplastics) can accumulate in our gut and other body tissues, we still know very little about them how they affect our health.
That’s partly because plastic particles have spread so quickly, going from obscurity to ubiquity in a few human generations.
As plastic products break down into smaller pieces over time, the particles can be incredibly durable and mobile, ultimately causing them to break down into small pieces seemingly everywhere on earth.
has microplastics permeated environments and food webs worldwide, from cities and farms to oceans and ice sheets. We eat, drink and inadvertently inhale them on a regular basis, and it’s estimated that the average person now ingests quite a lot 74,000 tiny plastic particles each year.
“We know that particulate plastic is ubiquitous in the environment and has been found in the human gut and other tissues like blood and even the brain and placenta.” says Study co-author Ying Chen, a biomedical engineer at Tufts University.
Microplastics are so widespread that scientists wanting to study their health effects on humans are now having trouble finding unaffected populations to serve as controls, the researchers note.
And while previous research has found one Link between microplastics and IBD, Evidence of a causal relationship remains difficult to find. Animal studies provide mixed results, showing accumulation of plastic particles in the gut and other tissues, but no clear-cut response to toxicity or inflammation.
So for the new study, Chen and her colleagues tried a different approach, using human gut organoids to see what microplastics might do in a real human gut.
“The use of organoids allows us to study the mechanisms of absorption and potential disease pathways in detail, which could help us understand the mixed results in the literature to date,” Chen said says“And have a more direct tissue model for potential impacts of plastic particles on humans.”
The researchers created their model of a human intestine on stimulus stem cells (which were derived from other organoids) to differentiate into the various cell types that occur naturally in the walls of the actual human gut.
They wanted a ratio of cells that resembled real gut walls in hopes of simulating the complex environment in which cells perform important functions such as absorption, hormone production, mucus secretion, and inflammatory responses, among others.
“It’s a significant advance over simpler cell models, which often included just one or a few cell types, some of which were derived from them Cancer Cells that may not show natural responses,” Chen said says.
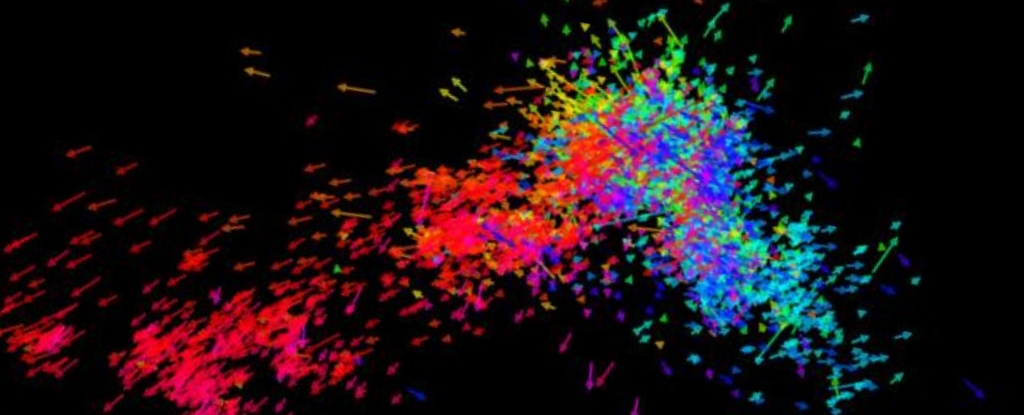
The experiments showed that different cell types absorb particles of different sizes. The smallest nanoplastics were taken up by epithelial cells that line the inner walls of the intestine microfold cells – which play a role in the immune response of the gut – absorbed larger particles and sent them to gut tissues.
The gut model was only damaged when microfold cells were present and higher concentrations of small plastic particles were present. According to the authors, the damage suggests that microplastics could contribute to the development of intestinal lesions.
The study found that higher amounts of nanoplastic also prompted the organoid to release inflammatory cytokines. These proteins are part of a normal immune response, but can also be play a role in conditions such as IBD when something upsets their natural balance.
Again, this only happened in the presence of microfold cells, suggesting they may help mitigate potential damage from microplastics in the gut.
Further research is needed to refine these findings and clarify how different types, sizes and amounts of microplastics can affect our gut. Nonetheless, this study offers a potentially valuable model for demystifying the danger.
“The results of this study suggest that using human cell organoids could be a powerful tool to better understand the potential toxicity of microplastics and nanoplastics, and environmental particles in general.” says Co-author David Kaplan, Professor of Engineering at Tufts University.
The study was published in nanomedicine.