The hair rising on the back of your neck, the gelid pool in the pit of your stomach, the flutter in your heart when a shadow shifts.
Fear can be devastating, sickening, and, strangely, a lot of fun. But it’s also an extremely useful emotion – an instinctive response to danger that can ultimately increase our odds of survival when situations take a turn for the worse.
There are times, however, when fear isn’t an appropriate reaction. In cases such as anxiety disorders and stress disorders, the fear response can become disproportionate to the situation or environment of the individual, seriously impeding mental health and quality of life.
In a bid to better understand fear and how it works, a team led by neurobiologist Hui-Quan Li of the University of California San Diego has mapped the changes in brain chemistry and neural signaling in mice receiving hefty frights – and, even better, figured out how to stop it.
“Our results provide important insights into the mechanisms involved in fear generalization,” says neurobiologist Nicholas Spitzer of UC San Diego.
“The benefit of understanding these processes at this level of molecular detail – what is going on and where it’s going on – allows an intervention that is specific to the mechanism that drives related disorders.”
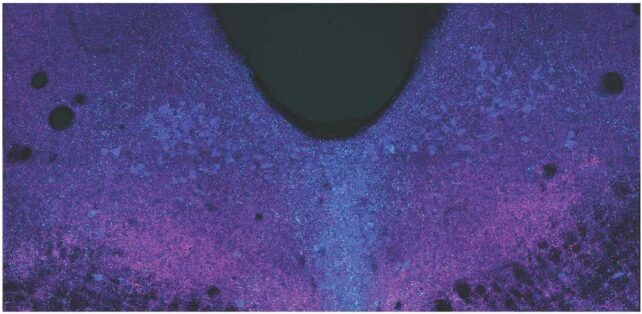
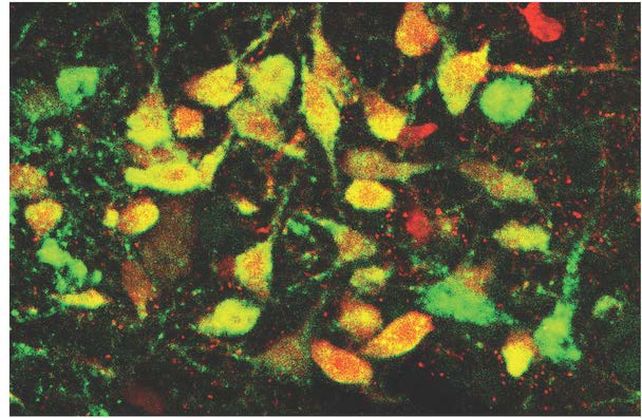
The study was conducted in mice genetically modified to express a specific transporter of the important neurotransmitter glutamate in the brain, as well as a fluorescent protein in the nuclei of their brain cells, to allow the team to track the changes in the brain.
The mice were given electric shocks at two different severities under specific conditions. When returned to that space two weeks later, mice tended to freeze in fear.
Those that received a strong shock also tended to freeze in a different environment, demonstrating an overgeneralized response. A look inside their brains showed what prompted this overzealous fear response.
Specifically, the researchers looked at a region of the brain called the dorsal raphe, located on the mammalian brainstem. This part of the brain is responsible for the modulation of mood and anxiety, as well as providing a substantial amount of serotonin to the forebrain.
The dorsal raphe also, importantly, plays a significant role in learning fear.
They found that a severe fright sort of flipped a switch in the neurons, changing the neurotransmission mechanism from glutamate, which excites neurons, to GABA, which inhibits neuronal activity. The switch appears to sustain a fear response where it would otherwise shut down or be absent, producing symptoms consistent with a generalized fear or anxiety disorder.
A study of the brains of deceased humans who had suffered from PTSD while alive showed the same switch from glutamate to GABA neurotransmission. This offered a starting point to figure out how to suppress the fear response.
One way was to inject mice with an adeno-associated virus that suppresses the gene responsible for making GABA. When the researchers trained these mice with the fear stimulus, they did not develop the signs of generalized fear disorder seen in the mice not treated with the virus.
That preventative method would require some foreknowledge of an ongoing stressor that could result in a disorder.
However, the researchers found a method of mitigating the effects of fear after the fact. If treated with the common antidepressant fluoxetine immediately after receiving a fright, the neurotransmitter switch and subsequent generalized fear were prevented.
But it had to be immediate. Administering the drug after the switch occurred, and the fear response was evident, was too late. The researchers say this could explain why antidepressants are often ineffective in patients with PTSD.
It’s not a cure, yet. But it’s a promising start down a path that could lead to effective treatment.
“Now that we have a handle on the core of the mechanism by which stress-induced fear happens and the circuitry that implements this fear, interventions can be targeted and specific,” Spitzer says.
The team’s research has been published in Science.





