The common artificial sweetener aspartame could be putting consumers at greater risk of heart disease through a newly discovered chemical trigger on the lining of arteries.
Researchers from Sweden, China, and the US gave mice doses of aspartame for 12 weeks, up to the equivalent level per day that a human would consume in about three cans of diet soda.
A number of the mice had been engineered to be missing a gene critical in metabolism, giving insulin unmitigated access to key receptors throughout their bodies.
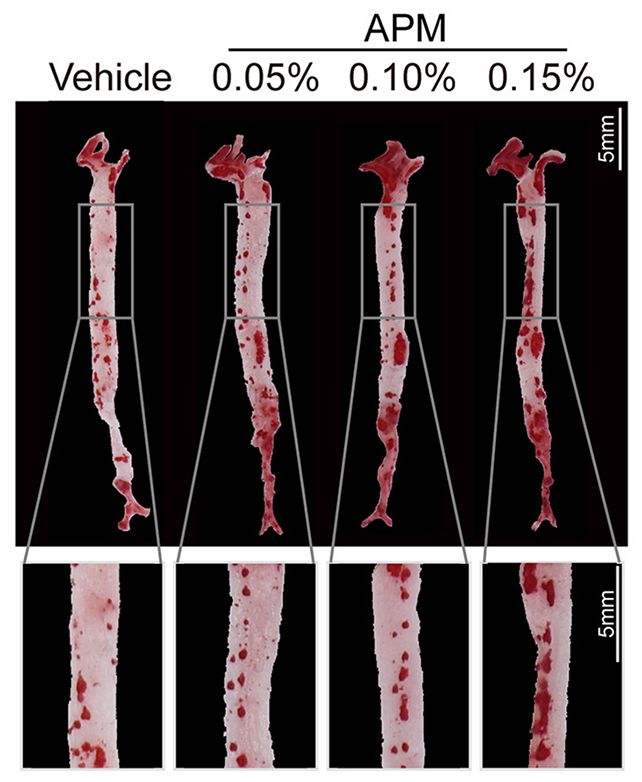
Compared with mice who hadn’t been fed the sweetener, the aspartame group had higher levels of insulin, greater blood vessel inflammation, and more fatty plaques in their arteries – all of which make a heart attack or stroke more likely.
“It is important to note that these findings have not yet been seen in humans,” explains cardiovascular physiologist James Leiper from the British Heart Foundation, who was not involved in the study.
“The results highlight the importance of further research to determine whether these additions to our food, and their effect on insulin levels, are contributing to an increased risk of cardiovascular events,” Leiper adds.
While artificial sweeteners have been linked to insulin interference before, there’s a lot we don’t know about the biological mechanisms at play or the subsequent health risks – which is part of the motivation behind this new study.
The researchers identified a signal molecule called CX3CL1 that became more active as insulin levels rose. Removing CX3CL1 receptors in the mice stopped the dangerous buildup of plaque in arteries – further evidence that this molecule is key to increasing the risk of heart damage in humans and could be targeted in treatments.
“Because blood flow through the artery is strong and robust, most chemicals would be quickly washed away as the heart pumps,” says vascular biologist Yihai Cao from the Karolinska Institute in Sweden.
“Surprisingly, not CX3CL1. It stays glued to the surface of the inner lining of blood vessels. There, it acts like a bait, catching immune cells as they pass by.”
The adverse effects seen in the aspartame-dosed mice are likely down to the sweetener being around 200 times sweeter than sugar – something that would send the receptors in the mouth and intestines into overdrive in terms of insulin production.
That would then lead to the impacts observed on vascular health and atherosclerosis – narrowed arteries – although future research will of course be needed to confirm the same chain reactions in the human body too.
“Artificial sweeteners have penetrated almost all kinds of food, so we have to know the long-term health impact,” says Cao.
While artificial sweeteners are often presented as healthier alternatives to sugar (which comes with its own problems), these substances have now been linked to cancer risk, increased anxiety, and learning issues in past studies.
That doesn’t mean avoiding artificial sweeteners in favor of sugar is best for our health. Chemist Oliver Jones from RMIT University in Australia notes in an expert reaction that he has “several concerns” about the study.
“If aspartame did cause some increase in cardiovascular risk (which this study does not prove), then that risk would likely be very small compared to things like high fat/high sugar diets and lack of exercise,” Jones says.
“In short, I don’t think this study itself gives us more reason to worry about diet drinks or aspartame.”
Given the number of factors involved, further investigation is needed. Though the experiments were on mice engineered to be more susceptible to insulin’s effects, the results highlight how boosted insulin levels can damage the lining of arteries.
“Understanding the mechanisms that underlie the exacerbation of atherosclerosis by artificial sweeteners is crucial for cardiovascular prevention and treatment,” write the researchers in their published paper.
The research has been published in Cell Metabolism.





