We already know that the virus behind cold sores, herpes simplex virus type 1 (HSV-1), can also infect the brain and the central nervous system, and now a new study sheds more light on how the viral attack spreads out.
Led by researchers from the University of Colorado and the University of Bourgogne in France, the study took a close look at the effects of the HSV-1 virus on the brains of mice, mapping out the different regions affected and assessing what the consequences might be.
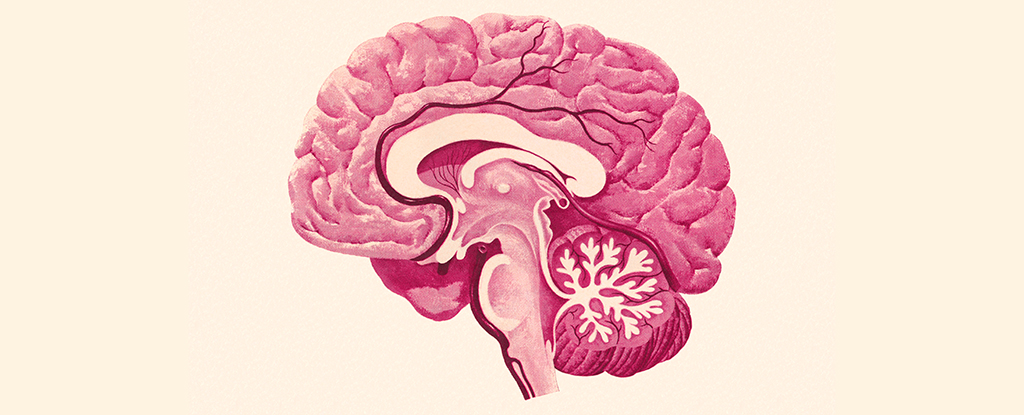
HSV-1 can be introduced to the central nervous system through two routes – the trigeminal nerve (through the face) or the olfactory nerve (through the nose) – although it remains unclear how the infection then spreads within the brain.
“Recently, this common virus has been implicated in neurodegenerative diseases, such as Alzheimer’s disease, but no clear route of central nervous system invasion has been established,” says neurologist Christy Niemeyer from the University of Colorado.
“Identifying how HSV-1 can get into the brain and what brain regions are vulnerable is key in understanding how it initiates disease.”
The team found that HSV-1 took hold in several of the brain’s most important regions, including the brain stem (responsible for co-ordinating heart and breath rate, along with sleep and movement), and the hypothalamus (which handles everything from sleep and moods to appetite and hormone levels).
However, other areas of the brain remained untouched by HSV-1 antigens, including the hippocampus (the region that looks after memory and special navigation, often connected to diseases like Alzheimer’s) and the cortex (linked to memory and attention).
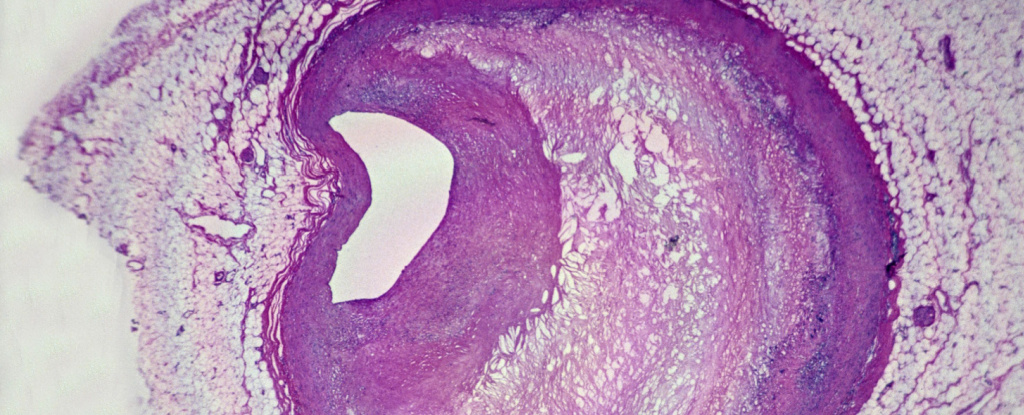
The researchers also looked at the activity of microglia (in-house immune cells of the central nervous system) in the mouse brains, which became inflamed when interacting with HSV-1. In certain regions, these immune cells stayed busy even after the virus had gone, suggesting ongoing inflammation.
In the most serious cases, HSV-1 can cause encephalitis, a life-threatening condition where inflammation affects the whole brain. While this didn’t happen here, the research shows there might still be damage being done.
“Even though the presence of HSV-1 is not causing full-blown encephalitis in the brain, it can still affect how these regions function,” says Niemeyer.
All of this additional knowledge gives scientists a better idea of how HSV-1 infections might be related to neurodegenerative diseases – something which has been the subject of several recent studies. The new study is another useful step forward that further research can now build on.
It’s been suggested that HSV-1 and microglia-related inflammation could be part of the reason why Alzheimer’s takes hold in some brains, or they may have some effect on its rate of progress. With that in mind, it’s interesting to see where there’s overlap in the brain regions affected by both HSV-1 and Alzheimer’s.
“Persistently inflamed cells can lead to chronic inflammation, a known trigger for a number of neurological and neurodegenerative diseases,” says Niemeyer.
“This research offers important takeaways in better understanding how viruses interact with overall brain health as well as the onset of pervasive neurological diseases.”
The research has been published in the Journal of Virology.