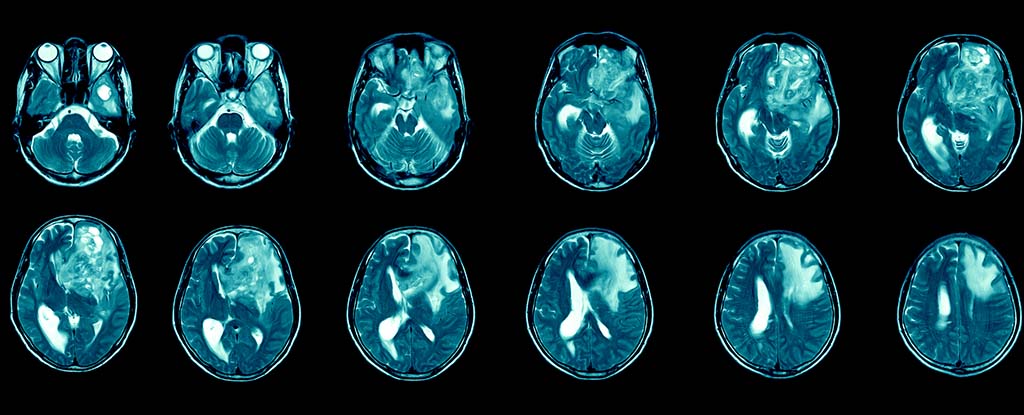
Glioblastoma is the most common and deadliest form of brain cancer. Patients face a bleak prognosis – the average survival after diagnosis is between 12 and 15 months. And just 6.9% of patients survive beyond five years, making it one of the most poorly survived cancers.
The toll this cancer takes goes beyond survival rates. Patients can suffer from symptoms like headaches, seizures, cognitive and personality changes, and neurological impairments. These symptoms may drastically affect their quality of life. But despite the urgent need, no targeted treatments exist for this devastating disease.
Researchers now believe that immunotherapy, which harnesses the immune system to target cancer cells, could be a turning point in the treatment of glioblastoma.
Glioblastoma is a naturally occurring tumour that belongs to a group of brain tumours called “gliomas” that originate and grow in the brain and spinal cord. Classified as a grade 4 tumour by the World Health Organization, glioblastoma is one of the most aggressive forms of cancer.
An estimated 3,200 new cases of glioblastoma are diagnosed each year in the UK, making up a significant portion of the 12,700 total brain and central nervous system tumours reported annually. Globally, there are approximately 3.2 to 4.2 cases per 100,000 people annually. This translates to around 150,000 new cases each year worldwide.
Standard treatments for glioblastoma – like surgery, radiation and chemotherapy – are often only temporarily effective. The tumours are highly resistant to these treatments due to the cancer’s ability to suppress immune responses and the presence of the blood-brain barrier, which restricts most drugs from reaching the brain.
After surgery, the tumour often returns and can spread to other parts of the brain. This leads to further challenges for patients and doctors alike.
Immunotherapy
The field of immunotherapy is evolving rapidly, with ongoing research expanding its potential applications across various diseases. Approved immunotherapy treatments are currently available for various cancers, like melanoma, breast and lung cancers.
Immunotherapy can also be used to treat autoimmune conditions like multiple sclerosis and rheumatoid arthritis, infectious disease like HIV and hepatitis B and C, and in allergic disease.
For the treatment of glioblastoma, immunotherapy represents a promising, though complex, avenue. Due to the tumour’s highly adaptive nature, glioblastoma presents different mutations in different regions of the brain. This makes it difficult to target. Even so, researchers are optimistic.
Recent trials have shown that immunotherapy can safely be delivered through injections into the cerebrospinal fluid. Scientists are now exploring how to adapt these methods to penetrate the tumour more effectively.
Despite the promise of immunotherapy, making it effective for glioblastoma remains a challenge. Funding shortages have hampered brain cancer research in the past. But new initiatives are helping to recruit researchers from other fields to tackle glioblastoma. This includes researchers like me.
For 20 years, I have studied how the immune system can be manipulated and modulated during cancer and chronic infection. More recently, I have studied how immune cells communicate and interfere with brain function which results in the onset of Alzheimer’s.
I am now applying that knowledge and experience to glioblastoma, where I’m investigating how to bypass the barriers that prevent treatment from reaching the tumours. My work is part of a global effort to develop and trial immunotherapy treatments specifically for glioblastoma.
While glioblastoma remains a complex and challenging disease to treat, immunotherapy offers a potential pathway to better outcomes for patients. But to date, there are no approved clinically available immunotherapies to improve the lives of patients with glioblastoma.
It’s also important to note that not all cancers respond to immunotherapy. And there may be immune-related side effects, such as organ inflammation. Careful consideration must be given to ensure that any treatment doesn’t result in swelling of the brain.
The delivery method of these drugs is also vital. Treating a patient with a simple injection into the arm and into the blood, or through the spinal cord, is better than having to perform surgery on the brain, for example. These considerations are a vital part of research.
The prospects for immunotherapy use in glioblastoma remain exciting, though. As interest and investment grow in the potential of immunotherapy, my fellow researchers and I remain hopeful that we may soon uncover more effective treatments for this terrible disease.![]()
Mathew Clement, Research Fellow at the School of Medicine, Cardiff University
This article is republished from The Conversation under a Creative Commons license. Read the original article.