Despite a wave of new and potential treatments for Alzheimer’s disease, diagnosing the condition before symptoms emerge and cognitive decline sets in remains a beastly challenge.
Understanding the root causes of Alzheimer’s disease – what causes brain cells to wither and die – is also proving more difficult to exact than everyone first hoped, though researchers are making progress wading through the possibilities.
Now a team from the US claims to have found in an animal study the ‘earliest-yet biomarker‘ that foreshadows the onset of this horrid disease before its characteristic amyloid-beta plaques take hold or any memory deficits are observed.
Even if that claim doesn’t immediately translate into a clinically useful diagnostic tool, the findings could help untangle one of the stranger clinical presentations of Alzheimer’s disease: elevated seizure-like activity.
It might seem counterintuitive at first, that a jolt in brain cell activity heralds a disease where neurons die and cognitive abilities fade. Past research has focused instead on the brain-wide slump in neuronal activity observed in Alzheimer’s disease, which tracks with cognitive decline.
But clinical studies have shown that in the early stages of disease, patients at risk of developing Alzheimer’s can experience a surge in neuronal activity in certain parts of their brains, detectable on brain scans before any symptoms appear.
In one study, nearly one-third of people carrying genetic variants predisposing them to Alzheimer’s disease experienced seizures. Another found people with Alzheimer’s who show sharp spikes in brain activity tend to be diagnosed at an earlier age.
This seizure-like activity could be linked to damage done to neurons before they deteriorate, with other processes hastening the decline.
The researchers behind this latest study wanted to trace this aberrant brain activity back to the cellular level, to figure out what mechanisms might trigger an overexcitability of neurons in the earliest stages of Alzheimer’s disease.
Other teams have pointed to a number of possible contributors, including abnormal levels of calcium ions inside cells and amyloid-beta (Aβ) plaques, one of the main hallmarks of Alzheimer’s disease.
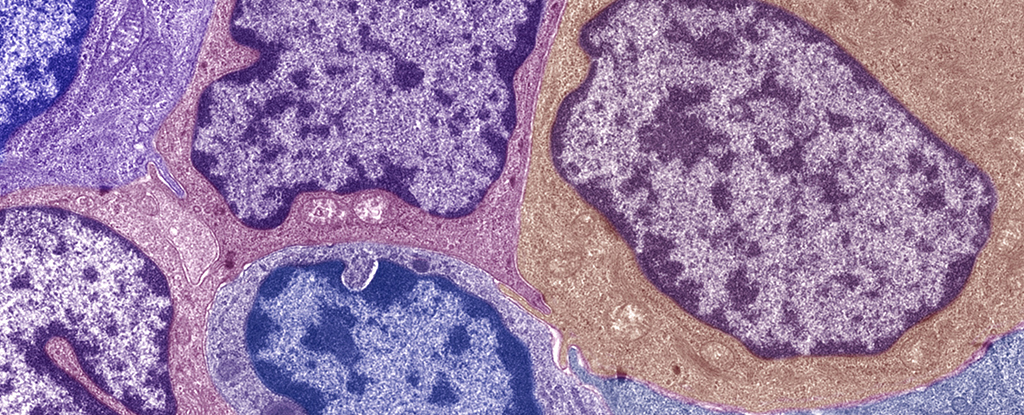
University of Illinois molecular biologist Yeeun Yook and colleagues landed on a protein specific to neurons called PSD-95, which promotes excitatory activity of synapses, the junctions between neurons, by recruiting more receptors.
In a series of mouse behavior and tissue experiments, the researchers found elevated levels of PSD-95, induced by the presence of Aβ, and showed how the protein was a driving force behind seizure activity. The animals were just 8 weeks old and had some Aβ in their blood plasma but no detectable plaques or memory problems.
Inhibiting PSD-95, the team saw reduced activity at the synapse and fewer seizures in mice.
“Our findings show that PSD-95 is a critical contributor to the hyperexcitability in the earliest stages of Alzheimer’s,” says Nien-Pei Tsai, a molecular biologist at the University of Illinois Urbana-Champaign and senior author of the study.
“So we think that PSD-95 can be an early biomarker to indicate that a patient could have Alzheimer’s disease or elevated seizure susceptibility.”
Of course, translating these findings into clinical applications will take a lot more work and is a long shot given Alzheimer’s ghastly track record. But the researchers are hopeful that PSD-85 could be a new target in Alzheimer’s disease.
“Validating this prediction may further strengthen our original hypothesis that PSD-95-dependent neuronal defects occur early in the disease and that inhibition of PSD-95, at least during the early phase of the disease, may slow down the progression of the symptoms,” the team concludes.
The research has been published in EMBO Reports.