More than a billion adults around the world live with increased blood pressurea condition that puts individuals at risk of damaging a variety of organs, including the nervous system.
Although previous studies associated with high blood pressure (Hypertension) With an increased risk of cognitive impairment, the mechanisms behind the deterioration in mental health have never been known.
An international team of researchers has now discovered which areas of the brain are most likely to be damaged when the cardiovascular system is under stress.
“Our study has for the first time identified specific locations in the brain that may be causally linked to high blood pressure and cognitive impairment,” says Mateusz Siedlinski, medical biologist at Jagiellonian University.
Siedlinski and colleagues used a combination of genetic and imaging data and observational analysis from 33,000 individual records in the UK Biobank to find the damage caused by high blood pressure, which contributes to dementia.
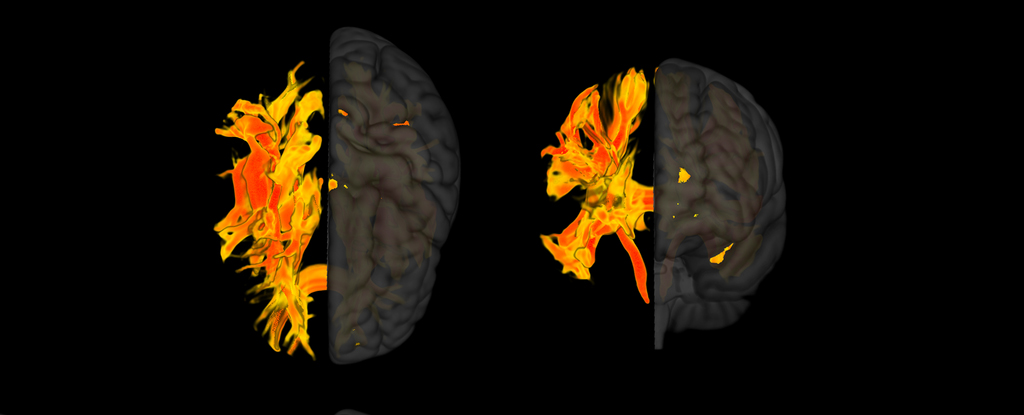
This combined approach allowed the researchers to identify where in the brain long-term high blood pressure can cause the structural changes that lead to a decline in cognitive function and what those changes look like in brain scan images.
“We thought that high blood pressure in these areas could impair cognitive functions such as memory loss, thinking ability and dementia.” explained Cardiovascular doctor Tomasz Guzik.
“When we verified our findings by examining a group of patients in Italy who had high blood pressure, we found that the parts of the brain we had identified were indeed affected.”
Previous studies had suggested links between total white matter and dementia, but non-cognitive function. The improved detail provided by the method of this new study showed that some white matter regions play a greater role than others in determining cognitive health, making broad measurements of the tissue an unreliable predictor of neurological impairment.
Focusing on specific parts of the white matter, Siedlinski and his team found changes in nine different areas that are linked to both high blood pressure and deterioration in brain function.
A section at the base of the forebrain, called the putamen, is essential to our responses to stimuli and learning. Other identified regions are involved executive functionDecision making and emotion regulation, and white matter pathways that act as communication channels between different brain regions.
In addition, the team found that structural changes were primarily a consequence of a difference between systolic pressure – the pressure in the arteries as your heart beats – and diastolic pressure – the pressure between beats. Higher systolic blood pressure and pulse pressure (systolic blood pressure minus diastolic blood pressure) influenced cognitive decline, while higher diastolic blood pressure appeared to have a protective effect when systolic blood pressure was taken into account.
This might explain Mixed results seen in previous studies which investigated possible links between blood pressure and cognitive decline.
The UK Biobank contains mostly data from middle-aged white people, so further research is needed to confirm that these results hold across different demographic groups. Nevertheless, the results give the researchers promising indications for further investigations.
“We hope that our results can help us to develop new ways to treat cognitive impairment in people with hypertension,” says guzik. “Studying the genes and proteins in these brain structures could help us understand how high blood pressure affects the brain and causes cognitive problems.
“Also, by looking at these specific brain regions, we may be able to predict who is more likely to develop memory loss and dementia associated with high blood pressure,” says Guzik continues.
“This could aid in precision medicine, allowing us to deliver more targeted therapies to prevent the development of cognitive impairment in the most vulnerable patients.”
This research was published in the European Heart Journal.