Deaths from cervical cancer are plummeting among young women in the US, and scientists think we have a single vaccine to thank for the numerous lives saved.
In the last decade alone, national health data suggests there has been a 62 percent drop in cervical cancer deaths in women under the age of 25.
Senior author Ashish Deshmukh, from the Medical University of South Carolina, attributes the dramatic change to the Gardasil vaccine.
His team’s research did not differentiate between young women who received the vaccine and those who did not, but Deshmukh says he and his colleagues “cannot think of any other reason that would have contributed to such a marked decline.”
Especially since studies in the UK and Australia have found cervical cancer rates are nosediving among those who have received the medicine.
The multi-dose Gardasil vaccine was approved for young girls in the US in 2006 to prevent deadly strains of the human papillomavirus (HPV).
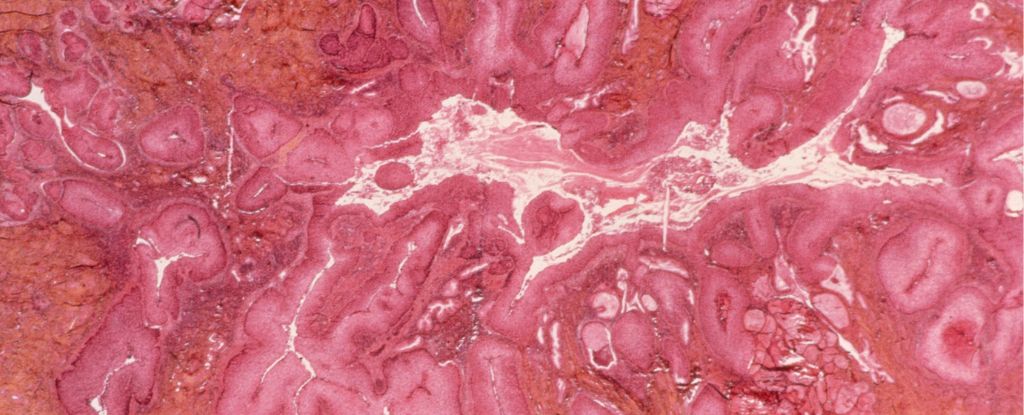
HPV is a highly infectious virus that can be transmitted through skin to skin contact, and it is responsible for 70 percent of invasive cervical cancers – one of the most common causes of cancer death among American women.
While it is rare for women to develop cervical cancer in their youth, new research suggests the vaccine is making cases under the age of 25 rarer yet.
According to national health data, the first cohorts of girls in the US who could receive the HPV vaccine (who were about 10 at the time) were far less likely to die from cervical cancer before the age of 25.
Previous studies in the US have shown that between 2012 and 2019, there was a 65 percent decline in cervical cancer cases among women under the age of 25. But this is the first study to consider death rates from those patients.
The research analyzed the health data of women under the age of 25 from 1992 to 2021 in three-year blocks.
Between 1992 and 1994, the US experienced 55 young cervical cancer deaths per 100,000 people.
Between 2019 and 2021, that number had dropped to 13 deaths per 100,000 people.
“The findings from this study highlight the urgency to improve HPV vaccination coverage,” conclude the authors.
In the US, HPV vaccination coverage among young girls reached 78.5 percent in 2021, but in the years since, that rate has barely improved, and even shows signs of slipping.
Australia has one of the highest vaccination rates for HPV in the world, at nearly 86 percent among girls, and by 2028, some national estimates predict there will be fewer than four new cases of cervical cancer per 100,000 people – a rate so low the disease could be considered eliminated.
In fact, a study in 2019 found that thanks to the HPV vaccine, cervical cancer could be eliminated in 149 out of all 181 countries by 2100.
But that’s only if vaccination rates are maintained and improved.
And it’s not just women whose lives can be saved. While the vaccine was first approved for young women, older women and boys and men can now also receive the HPV vaccine, as it has been found to protect against anal, penile, and oral cancers.
The HPV vaccine promised a lot, and it’s lived up to the challenge. The medicine is now saving far more lives than scientists ever thought possible, turning some of the most deadly diseases into preventable ones.
The study was published in JAMA.